


|
Uveitis
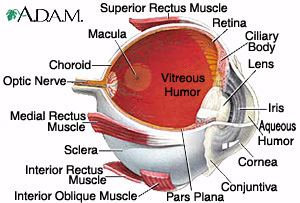
The eye is a hollow, fluid filled, three layered ball, of tissue. The outermost layer is the Sclera (white coat of the eye), the middle layer the Uvea, and the innermost layer is the Retina (thin light-gathering layer).
Uveitis
Uveitis or Intra-Ocular Inflammation or Ocular Inflammatory Disease is inflammation of the Uvea Tract, middle section of the eye. Uvea Tract has three parts: the Iris (the colored part of the eye), Ciliary body (behind the iris, responsible for manufacturing the fluid inside the eye), and Choroid (the vascular lining tissue underneath the Retina). The Uvea Tract is the structure responsible for the eye's blood supply. Inflammation of the Uvea can affect the Cornea, the Retina, the Sclera, and other vital parts of the eye. Since the Uvea borders many important parts of the eye, inflammation of this layer may be sight-threatening and more serious than the more common inflammations of the outside layers of the eye. Uveitis is the third leading cause of blindness in this country.
Anterior Uveitis
Anterior Uveitis, Iritis, or Iridocyclitis is inflammation that affects the front of the eye, the Iris which is Iritis or Nongranulomatous Uveitis, or the Ciliary body which is Iridocyclitis. The Iris is the colored part of the eye which contains the Pupil. The Iris is a muscle which dilates or constricts the Pupil, letting light enter into the eye. Behind this is the Ciliary body a circular structure, which produces the clear fluid (Aqueous Humor) which fills the eye, passing through the Pupil and draining away near the edge of the Iris. Ciliary also contains the Ciliary muscle attached to the lens responsible for changing the shape to focus.
Symptoms
Redness, pain, photophobia (sensitivity to light), blurred vision. The Iris may adhere to the Lens, thus increasing the intraocular pressure. There may be nodules on the Iris. Tearing and the Pupil may be constricted and nonreactive. In severe cases of Anterior Uveitis, there may be hypopyon (a small amount of pus or collection of white cells).
Intermediate Uveitis
Intermediate uveitis, Middle Uveitis, Cyclitis, Pars Planitis, Peripheral Uveitis, or chronic Cyclitis is inflammation that affects Ciliary between Anterior and Posterior Uvea which can also affect the Vitreous and Retina. There have been some implications of an association with Sarcoidosis, Lyme disease, Juvenile Rheumatoid Arthritis, and Multiple Sclerosis (MS). There are exacerbations and remissions and typically this disorder runs a very long course. Inflammatory mediators will increase vasopermeability of Retinal capillaries resulting in posterior segment inflammatory cells as well as Cystoid Macular Edema (CME). Vision loss occurs due to Cataracts and CME.
Symptoms
Painless, blurred vision, floaters.
Posterior Uveitis
Posterior Uveitis, also known as Choroiditis, Granulomatous Uveitis, is inflammation that affects the part of the Uvea at the back of the eye. The Choroid is basically a layer rich in small blood vessels and connective tissue which supplies the inner parts of the eye. The inflammation may affect, the Retina (Retinitis, Chorioretinitis)in the blood vessels at the back of the eye (Vasculitis), and Optic Nerve. Cells may be seen in the Vitreous Humor, (transparent gel that fills the eyeball behind the Lens). Yellowish or dark areas of inflammation on the Choroid and the Retina. The blood vessels in the Retina develop a sheath or covering of inflammatory tissue.
Symptoms
Decreased vision, distortion of the size or shape of objects (Metamorphopsia), floaters, pain if Optic nerve is involved, photophobia. The resulting scars may impair clear vision and cause dimness of vision (Amblyopia).
Vision can be impaired suddenly or gradually reduce over time.
Diffuse Uveitis
Diffuse Uveitis Panuveitis, or Endophthalmitis is inflammation involving all parts of the eye, including Anterior, Intermediate, and Posterior structures.
Symptoms
Diffuse Uveitis may produce any or all of the above-mentioned symptoms.
Cause
Uveitis has many different causes. It may result from a virus, a fungus, a parasite, or injury to the eye. Chronic Uveitis is often related to an Autoimmune Disorder.
Treatment
Uveitis is treated by an ophthalmologist (Uveitis specialist). Uveitis is usually treated with both a topical eye solution and an oral medication containing corticosteroids. Nonsteroidal anti-inflammatories such as ibuprofen may be used for pain relief. Treatment systemically, that is, the underlying disorder must be controlled in order to halt the progression of the eye disease. This usually requires systemic steroids (e.g., prednisone) during acute stages, and immunosuppressive agents are often required for long-term control.
Complications
Ocular complications of Uveitis may produce profound and irreversible loss of vision, especially when unrecognized or treated improperly. The most frequent complications include Cataracts, Glaucoma, Glaucomatocyclitic Crisis, Retinal detachment, Neovascularization of the Retina, Optic Nerve, or Iris and Cystoid Macular Edema, the most common cause of decreased vision from Uveitis. Patients suspected of having Uveitis should, therefore, be referred immediately for complete ophthalmologic evaluation.
Links to References,
Ocular, and Immunologicial-Vasculitis Help
Uveitis Specialist
Massachusetts Eye& Ear Infirmary
St Lukes Eye
Uveitis Iformation Group
Uveitis Support
EMedicine
IntellHealth
Merck
HEALTHCENTRAL
Handbook of Ocular Disease
Cleveland Clinic Immunologic Disease Center
Cole Eye Institute
John Hopkins Vaculitis Center
John Hopkins
Wilmer Eye Institute
National Eye Institute
Disclaimer: I'm not a doctor nor do I play one on TV!!!
 Copyright © 2002-2006 LMK
Copyright © 2002-2006 LMK
|




|